States moving faster than feds on ending unfair billing practice
TULALIP, Wash. — Gov. Jay Inslee signed into law on Tuesday new ambulance surprise billing protections, making Washington the 16th state to enact such a statute. The bill moved quickly through both houses of the state legislature with nearly unanimous approval after its first public hearing on January 12. Ambulance companies across the country have a history of sending surprise bills — out-of-network bills that insurance doesn’t cover, from a provider a patient didn’t choose or couldn’t avoid. Out-of-network providers deliver about 50 percent of ambulance rides.
Beginning January 1, 2025, Washington’s new state law will prohibit out-of-network ambulance companies from sending a surprise “balance bill” to patients who receive emergency medical treatment at the scene or are transported to an appropriate emergency service provider’s location. The law clarifies that patients need only to pay their cost-sharing amount as if the service was provided by their insurance company’s in-network providers. To ensure ambulances receive adequate reimbursement, the new law requires health plans to pay the ambulance company the amount set by the local government. If no such local government rate exists, then the plan must pay the lesser of: 325% of Medicare rates or what the ambulance charged. The law applies to patients who are insured by state-regulated insurance plans.
“Many patients in Washington will no longer need to fear unknowable, expensive surprise bills from ambulances the next time they experience a medical emergency,” said Patricia Kelmar, PIRG’s Health Care Campaigns senior director. “We applaud the swiftness with which Washington studied and addressed this gap in surprise billing protections.”
During the first public hearing, Christy Shum described her billing nightmare when her newborn needed sudden transportation to a nearby children’s hospital. She and her husband didn’t know that the local hospital had called an out-of-network ambulance, so they owed $6,000 of the $7,000 bill.
The federal, bipartisan-supported No Surprises Act, which took effect on January 1, 2022, protects patients from out-of-network bills for care in emergency rooms and in-network hospitals and for transportation by air ambulances. The federal law excluded ground ambulances from the ban on surprise bills and instead established a Ground Ambulance and Patient Advisory Committee, which included Kelmar, to make recommendations to Congress. We expect the report from that federal committee within the next three months.
Meanwhile, states aren’t waiting for a federal solution. In 2023, four states passed ambulance surprise billing protection laws, bringing the total to14 states. In the last week, two more states have enacted state legislation: Washington and Indiana, where Gov. Eric Holcomb signed its bill on March 13. While state laws help some insured patients, a federal solution is necessary to extend ambulance surprise bill protections for those enrolled in employer-sponsored insurance plans.
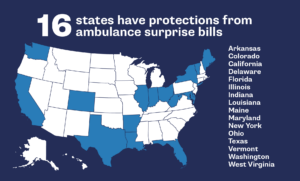
As of March 19, 2024, sixteen states have passed ambulance surprise billing protectionsPhoto by TPIN | TPIN
***If you want to speak to a Washington state resident who has received an ambulance surprise bill, please contact Patricia Kelmar at 609-651-7654 or [email protected] for a connection.***