Nursing home safety during COVID: Staff shortages
Facilities struggled with staffing even before the pandemic; 23 percent reported shortages by year's end
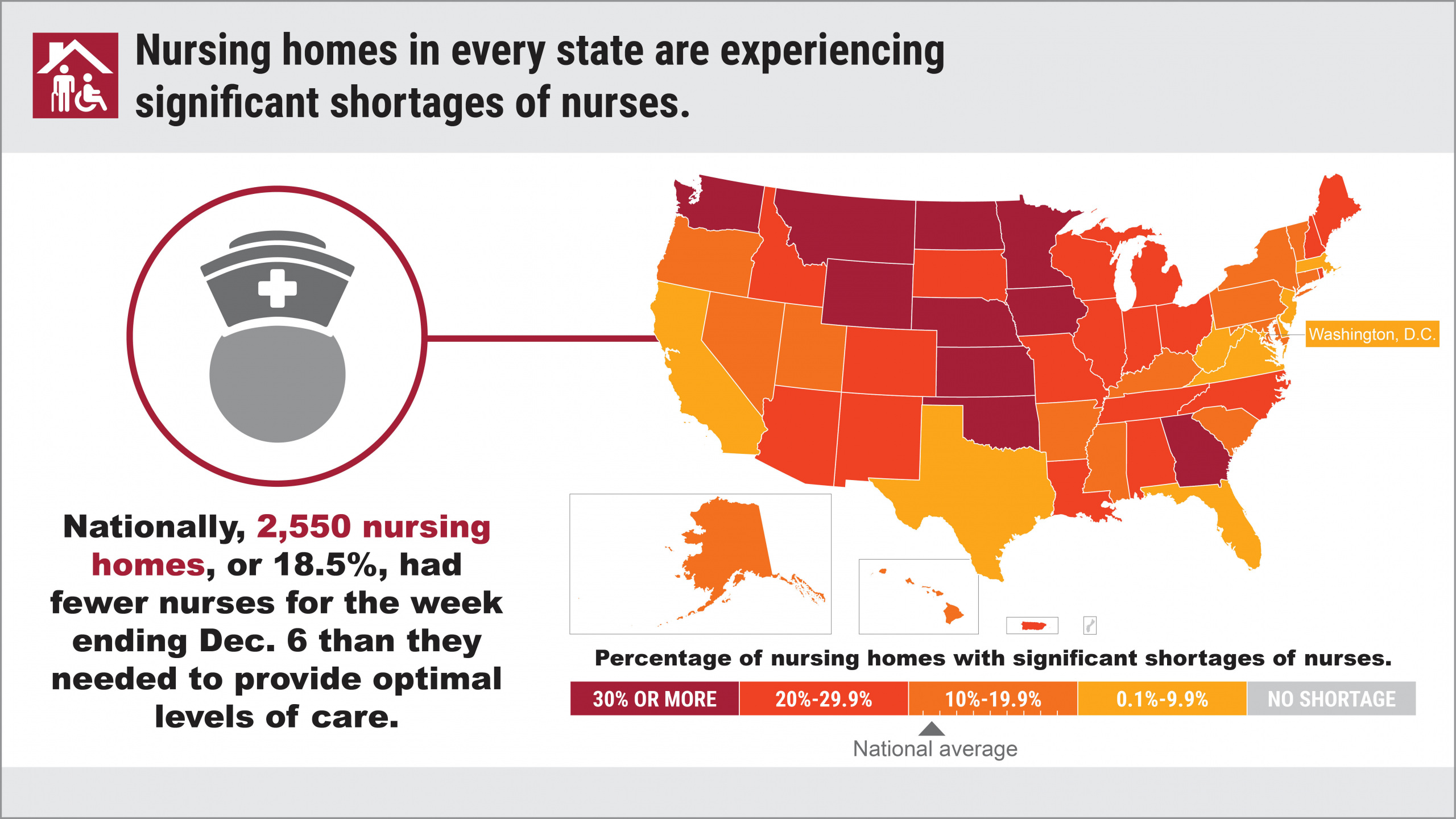
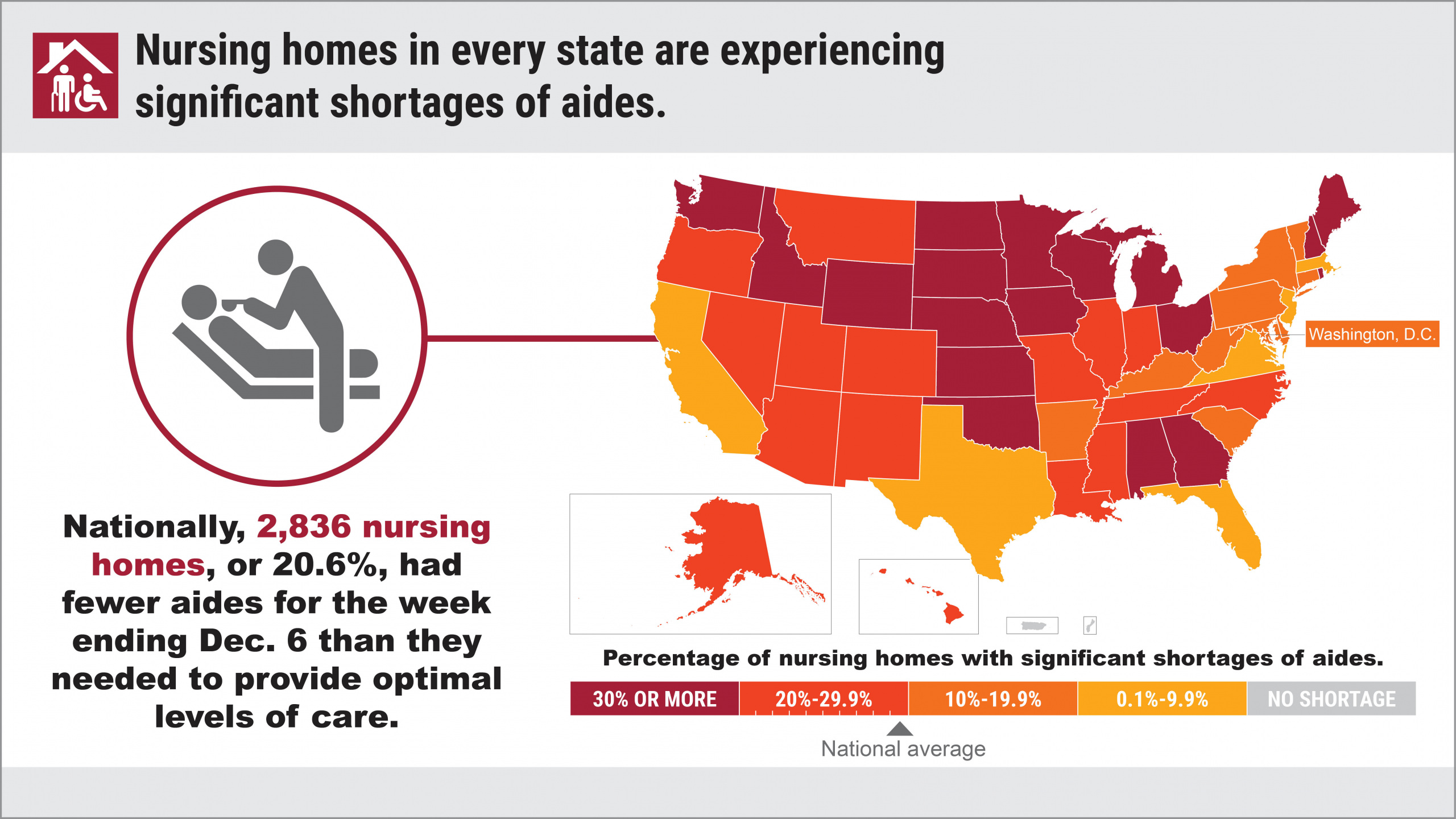
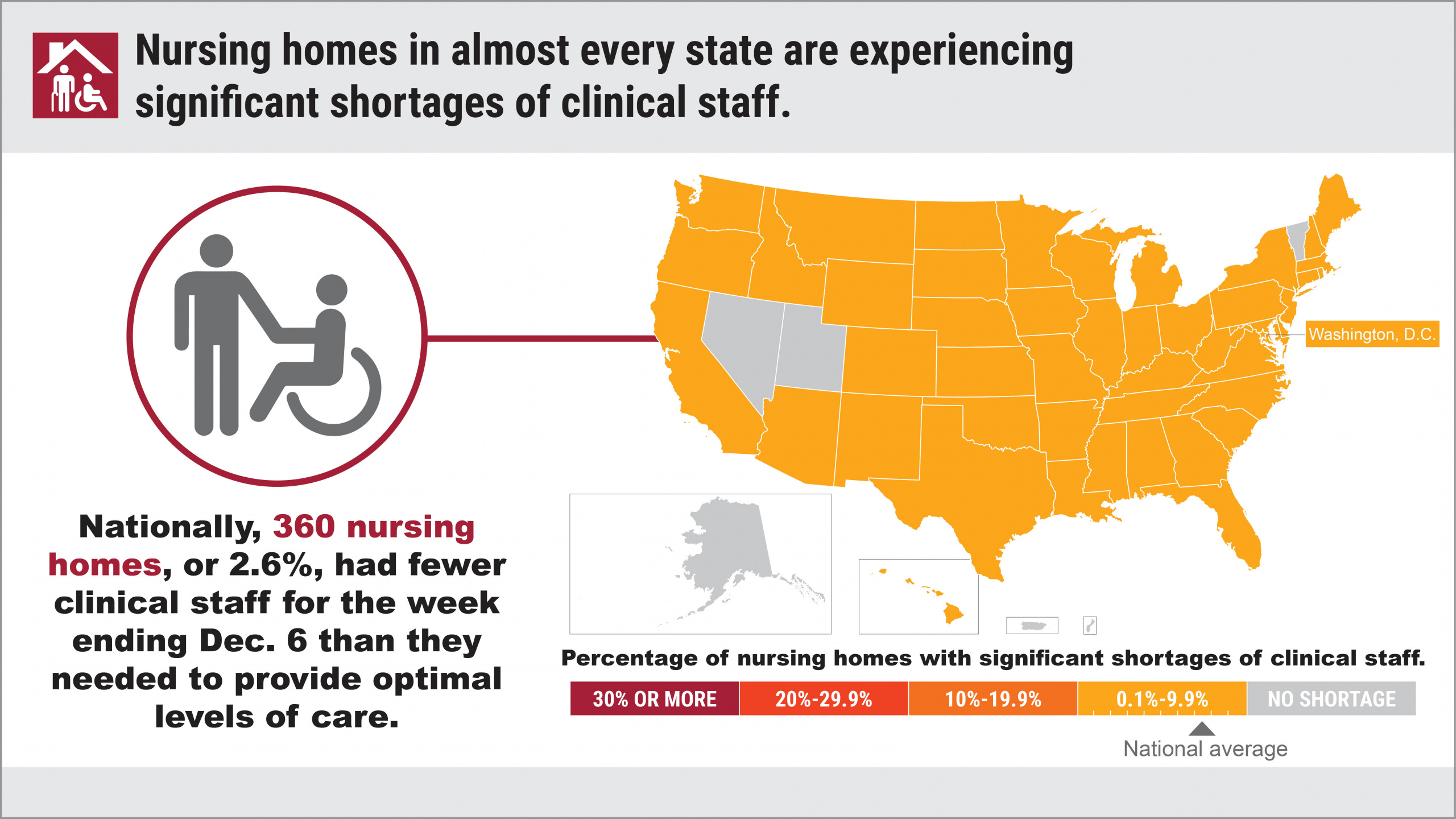
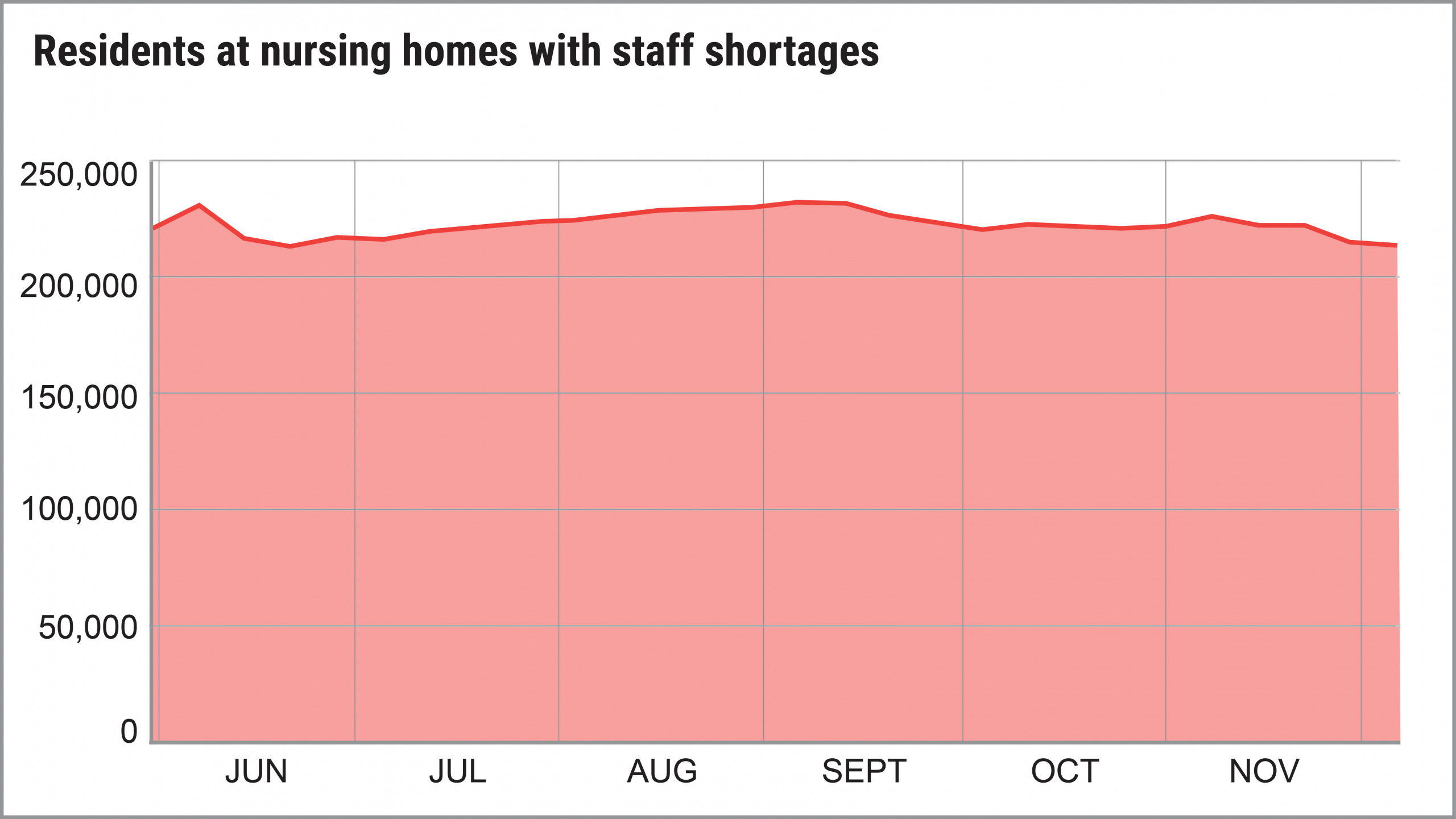
More than 3,000 U.S. nursing homes last month had a shortage of nurses, aides or doctors, and it’s a severe problem that has existed since last May. For most of last year, more than 200,000 people at any given time were in nursing homes that themselves acknowledged they were suffering from staff shortages.

A report created as part of a series by U.S. PIRG Education Fund and Frontier Group
By Teresa Murray, U.S. PIRG Education Fund,
with data analysis by Jamie Friedman, Frontier Group
VIEW THE REPORT
More than 3,000 U.S. nursing homes last month had a shortage of nurses, aides or doctors, and it’s a severe problem that has existed since last May. For most of last year, more than 200,000 people at any given time were in nursing homes that themselves acknowledged they were suffering from staff shortages.
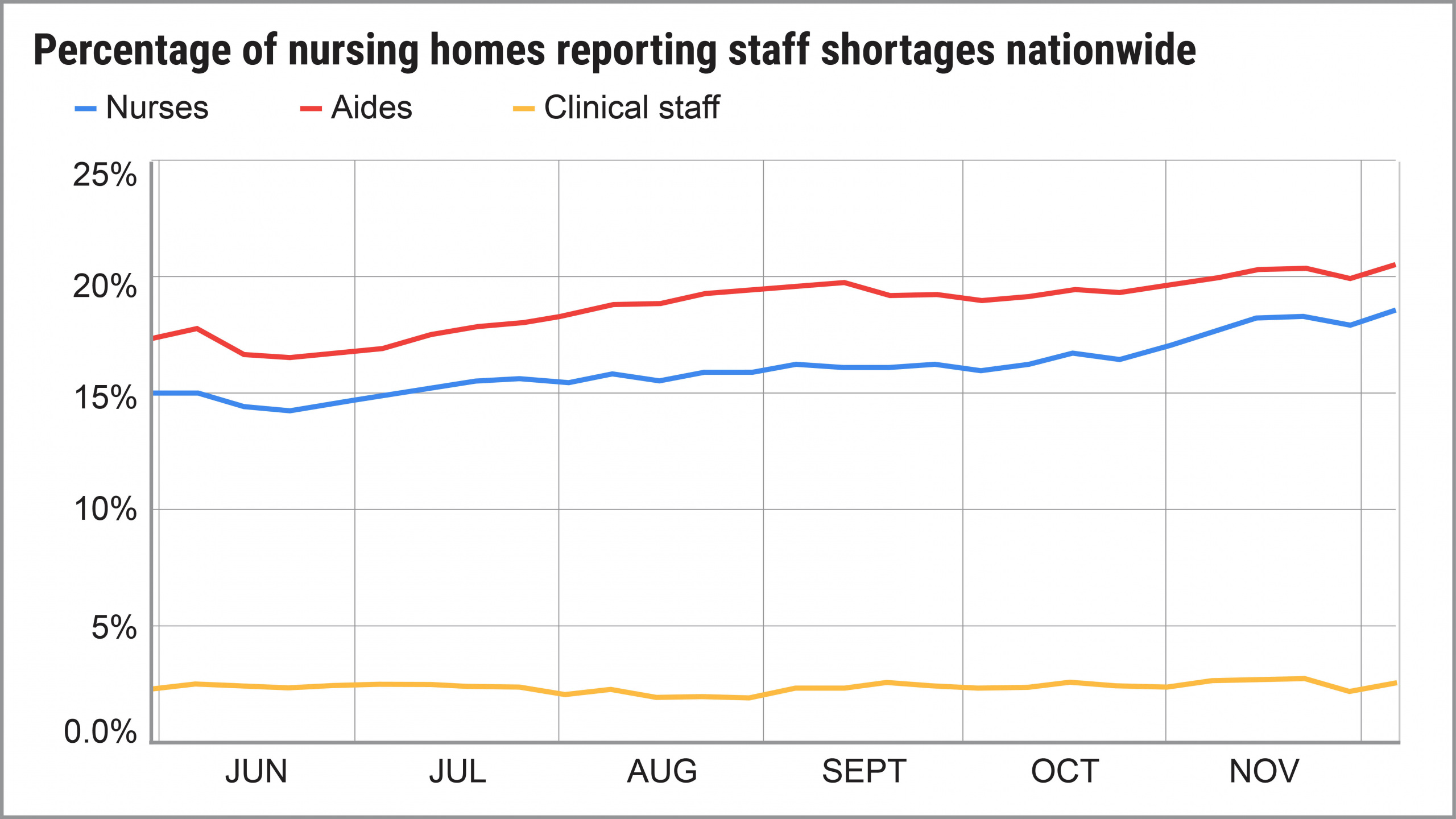
In fact, the number of homes reporting shortages of nurses, aides or clinical staff actually increased from May to December, according to an analysis of government data by U.S. PIRG Education Fund and Frontier Group. By early December, 23 percent of homes reported a shortage of at least one category of direct-care staff.
Not only are the shortages a direct result of the COVID-19 pandemic, experts say, but in a circular nightmare, the staff shortages also fueled more COVID outbreaks in nursing homes among residents and staff. More cases mean more stress for workers and more workers who contract the virus or are exposed, which then leads to even more staff shortages. The end result: In many cases, when there aren’t enough workers, patient care suffers.
Key findings
At any point in time, there are about 1.3 million people with short-term rehabilitation needs or long-term illnesses who reside in the nation’s 15,000 nursing homes. During the period we examined, from May 31 through Dec. 6, shortages of nurses and aides grew more dire as the year went on:
Consequences of staffing shortages
Why staff shortages got worse
How nursing homes are coping with shortages
What needs to be done
Find out more
Video guides
How to look up all nursing homes in a particular city, zip code.

Topics
Find Out More


Nursing home safety during COVID: Cases and vaccines

Nursing home safety during COVID: Cases and Vaccines