Deirdre Cummings
Legislative Director, MASSPIRG
617-747-4319
[email protected]
Legislative Director, MASSPIRG
617-747-4319
[email protected]
Report: Nursing homes endure massive PPE shortages
Seven months into COVID-19 pandemic, Massachusetts’ nursing homes still at risk
Boston— Massachusetts nursing homes, along with thousands nationwide, have dangerous shortages of masks, gowns and other items they need to protect residents, workers and the broader community from COVID-19. When nursing homes don’t have enough personal protective equipment (PPE), it leads to outbreaks among residents and staff, worker quarantines and shortages, and more risk to workers’ and residents’ families and neighborhoods.
Massachusetts has had more than 6,000 deaths in long term care facilities which include nursing homes, rest homes and assisted living facilities, accounting for more than sixty percent of the confirmed COVID-19 deaths in the state.
In the spring, outbreaks in nursing homes made state and national headlines. Now, seven months into this pandemic, PPE shortages have become much worse, according to “Nursing Home Safety During COVID: PPE Shortages,” a report by MASSPIRG Education Fund and Frontier Group. Our analysis of data submitted to the Centers for Medicare & Medicaid Services from May through August of 2020 by the nation’s 15,000 nursing homes shows:
● There were 226,495 residents at risk nationwide in August because they were in homes that were out of or were dangerously low on one or more types of PPE such as N95 masks, gowns or hand sanitizer.
● Eight percent of nursing homes were completely out of one or more types of PPE in late August; 20 percent of facilities had less than a one-week supply of one or more types of PPE, which represents a critical shortage by industry standards.
● In May, 2 to 4 percent of homes were totally out of N95 masks, surgical masks, gowns and eye protection. That improved in June, but shortages started soaring in mid-July and more than tripled by late August.
● In 20 states, at least 20 percent of nursing homes were out of or critically low on N95 masks in August. At least 10 percent were out of or critically low on gowns in 26 states
In Massachusetts, 360 nursing homes with a 40,000-bed capacity were included in the national review. The findings are concerning, as Massachusetts, like much of the rest of the country is now experiencing significant increases in COVID-19 cases.
● In Massachusetts, the shortages of N95 masks, surgical masks and eye protection increased significantly in the first half of July and remained at roughly the same levels through August. Massachusetts has had double-digit shortages of gowns throughout the 3 months.
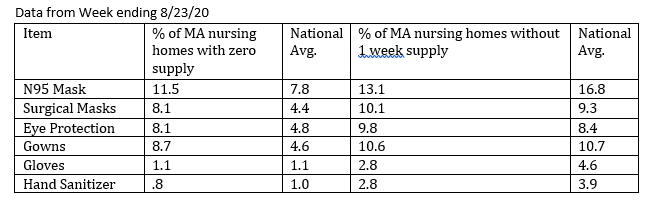
● During the week of 8/23/20, about one in 10 Massachusetts nursing homes had a less-than-one-week supply of N95, surgical masks, eye protection and gowns and more than 1 in 13 homes had no supply. The state was faring better on gloves and hand sanitizer, with 1 in 40 having a less-than-one-week supply, and 1 in 100 having no supply.
“It’s unconscionable that we are dealing with any PPE shortages at this point in the pandemic, especially in nursing homes where the most vulnerable are exposed and where the disease can spread quickly in and out of the facilities,” said Deirdre Cummings, MASSPIRG’s Consumer Program director. “Among the findings, I’m most concerned that we have too many nursing homes reporting they have no N95 masks, surgical masks, eye protection and/or gowns. We can and must do better,” Cummings said.
“It is alarming that there continue to be nursing homes in Massachusetts that do not have a sufficient supply of personal protective equipment to ensure the safety of their residents, said State Representative Ruth Balser, House Chair, Joint Committee on Elder Affairs. “I am glad to hear the Administration is building its stockpile and I further call on them to establish an exchange to facilitate the purchase of PPE for nursing homes. As we watch the numbers of cases increase again, we need to do everything we can to protect these most vulnerable residents of Massachusetts, those who live in our nursing homes.”
Cummings added that experts believe PPE shortages have continued to get worse. One group, GetUsPPE, a grassroots movement founded by medical professionals on the COVID frontlines, said more facilities across all sectors were complaining of shortages in September.
Medical experts believe the shortage of PPE is a key reason that outbreaks and deaths from COVID-19 are disproportionately high in nursing homes. This issue becomes even more urgent with talk of a “herd immunity” strategy that would allegedly safely cordon off nursing home residents and other at-risk populations while COVID tears through the rest of society. In reality, evidence suggests that until we have a vaccine, without a stronger adherence to spread-prevention practices that usually involve PPE, infection will likely run rampant.
In the report, MASSPIRG calls for a number of policy actions to improve the supply and transparency of availability of PPE. Those actions include: the federal government fully implementing the Defense Production Act so more PPE is available and sold at reasonable prices; congressional action to streamline the supply chain; and multi-state consortiums to reduce competition and stabilize prices.
In Massachusetts, Governor Baker and the Coronavirus Command Center, have made significant investments to protect residents, staff and the community in and around our long-term care facilities including securing PPE. The Commonwealth’s Health and Human Services Secretary Marylou Sudders testified before the House Ways and Means Committee last week that, “based on the PPE we have now and shipments we expect this fall, we have sufficient PPE to support the emergency supply needs of health care and human service providers and first responders from now until the end of 2021.” In addition, the state has set up a hotline for nursing homes in need of securing PPE.
The PPE shortage is among the problems brought to light by the CMS data on nursing homes. We will explore various issues in a series of reports in the months ahead.
MASSPIRG released a consumer guide on what to ask nursing homes to make sure they are safe, and a video that illustrates how to use the CMS database to find out COVID information about nursing homes.
****
MASSPIRG Education Fund is an independent, non-partisan organization that works for consumers and the public interest. Through research, public education and outreach, we serve as counterweights to the influence of powerful special interests that threaten our health, safety or well-being.