
EMERGENCY: The high cost of ambulance surprise bills
Half of ambulance rides by insured patients could result in a surprise bill. We need a solution now.

Download the full report here
UPDATED 3/24/2024: Since this report was issued, in 2023, four additional states passed patient protections from ambulance surprise bills (Arkansas, California, Louisiana, and Texas). And as of March 19, 2024, two new states have enacted their own ambulance surprise billing protections (Indiana and Washington). There are now 16 states with state-based ambulance surprise billing protections. Please disregard the chart on p.8 in the downloadable PDF. The image below is now accurate.
When a medical emergency strikes, the most important thing is to get help fast. And about 1 in 10 times, insured Americans get to the emergency room by ambulance. In fact, ground ambulances transport approximately 3 million privately insured people to emergency rooms annually.
The problem is that patients generally don’t choose their ambulance service. They (or someone else) call 9-1-1, and the dispatcher sends out a responder. Then, the patient is obligated to pay the bill.
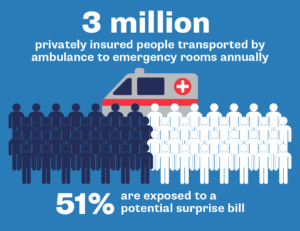
Photo by TPIN | TPIN
In December 2020, Congress passed the No Surprises Act (NSA) to protect patients from many types of out-of-network balance bills. The law prohibited surprise billing for emergency room services, air ambulances and most out-of-network care at in-network facilities.
It did not include protections from surprise billing by ground ambulances.
Yet, Congress acknowledged important work was left undone, by including provisions in the NSA to establish the Advisory Committee on Ground Ambulance and Patient Billing. The committee is charged with reviewing options for protecting consumers from surprise ground ambulance billing.
Studies show about half of emergency ambulance patients with insurance are at risk of receiving a surprise medical bill which is an out-of-network charge for those transportation services. Those balance bills carry a median out-of-pocket charge of $450 but in some states, the average is more than $1000.
Balance billing occurs when patients are charged the difference between the in-network and out-of-network rate. This common billing practice throughout the health care industry is even more prevalent for ambulances.
Ambulances have the highest out-of-network billing rate in the country, adding up to around $129 million spent by insured patients on ambulance surprise bills every year. In at least seven states, more than two-thirds of emergency ground transports could result in a balance bill.
As of October 2023, 14 states have enacted laws to protect patients against out-of-network bills from ambulance companies. However these state laws are limited to protecting only patients who are insured by a state-regulated health plan. That means that 60% of those who get their insurance coverage through a self-funded plan offered by their employer are left unprotected because these types of plans are exempt from state laws. Insured patients need a federal solution, modeled after these state laws, to ensure protection across all 50 states.
This report highlights the need for nationwide ground ambulance surprise billing protections. It provides an overview of the ground ambulance business models and how states have addressed the problem of ambulance balance billing. In addition, it recommends what data the government should accumulate and what policy solutions the government should consider based on that data.
Download the full report at the button above.
Share your ambulance story here.
Topics
Authors
Patricia Kelmar
Senior Director, Health Care Campaigns, U.S. PIRG Education Fund
Patricia directs the health care campaign work for U.S. PIRG and provides support to our state offices for state-based health initiatives. Her prior roles include senior policy advisor at NJ Health Care Quality Institute, associate state director at AARP New Jersey and consumer advocate at NJPIRG. She was appointed to the Ground Ambulance and Patient Billing Advisory Committee in 2022 and works with patient advocates across the U.S. Patricia enjoys walking along the Potomac River and sharing her love of books with friends and family around the world.
Find Out More

Outpatient outrage: Hospitals charge fees for care at the doctor’s office

A bad deal: Why you don’t want (medical credit) cards in your hand
Medical Bills: Everything you need to know about your rights
