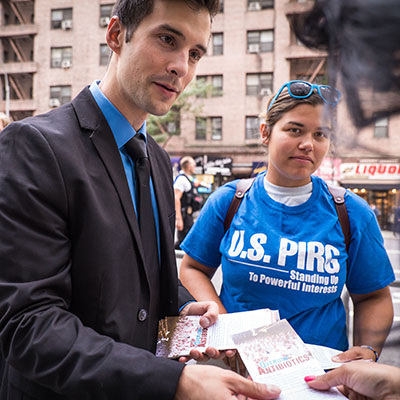
Matt Wellington
Former Director, Public Health Campaigns, PIRG
Public Health Campaigns Director Matt Wellington and Dr. Syra Madad detail how people can safely gather this holiday season in the era of COVID-19.
Former Director, Public Health Campaigns, PIRG
By Matthew Wellington, U.S. PIRG Public Health Campaigns Director and Dr. Syra Madad, Sr. Director, System-wide Special Pathogens Program, NYC Health & Hospitals
A holiday dinner can create memories you’ll have for a lifetime, such as your grandfather talking about how he and your grandmother first met, sharing laughs with siblings who you haven’t seen all year, or just the comfort of enjoying a good meal together.
Most years, Americans start making holiday travel plans around now, but with the COVID-19 pandemic worsening again, millions of families across the country are starting to wonder what the holidays will look like this year.
We can still make memories this holiday season, but they will look different than our lives before COVID-19. And whether we can safely gather with family at all depends on several factors, including the rate of transmission of COVID-19 in your area, precautions that you take before and during the holiday gathering, and whether we have better testing infrastructure to detect cases early.
While a handful of states currently have the virus under control, it continues to spread unchecked in much of the United States. There’s no silver bullet to get us out of this mess, but widespread testing coupled with ongoing preventative measures could certainly give us some pieces of our lives back. Currently, we’re testing primarily to diagnose if someone has COVID-19, and to track and test close contacts or those who might have been exposed. The most prevalent type of test being used is molecular, which has significant supply chain hurdles and long turn-around-times.
If we want to see our families or attend religious services for the holidays without fear of contracting or spreading the virus, we need to abide by and normalize preventative behaviors such as mask-wearing, dramatically increase the amount of testing we are doing across the country, and offer testing not just for diagnostic purposes but also for screening purposes. Screening tests for SARS-CoV-2 are used to identify asymptomatic or pre-symptomatic people and prevent the spread of the virus.
Currently the United States is administering around 1 million COVID19 tests per day. To contain and track the virus, prevent widespread community outbreaks and reopen the economy safely, the U.S. needs at least 14 million tests per day for screening.
Massachusetts has hit its testing target, and a few other states are close to testing enough people to effectively suppress the virus. Connecticut, for example, is providing widespread access to testing sites with the ability to return results within 24 to 48 hours. It has also made information on testing locations easy to find online, launched an ad campaign to educate people about how and when to get tested, and dispatched mobile testing facilities to high risk areas. Maine implemented similar testing strategies and now has one of the lowest virus levels in the country.
The federal government announced recently that it plans to deliver 100 million rapid tests to states. That’s good, but nowhere near what we need. It’s up to state governors to make it happen, and they can do so by borrowing best practices from successful states. States can boost test purchasing power by joining a consortium with other governors, similar to the one started by Gov. Larry Hogan in Maryland and the National Governors Association. They can improve their testing capacity by increasing the number and variety of testing locations, and by mobilizing a local network of labs, as New York did. Targeting testing at higher-risk settings such as churches, nursing homes, meat-packing facilities and schools is also important.
If we ramp up our testing capacity, continue preventative measures, and track and trace through a well coordinated contact tracing infrastructure, you might be able to see your family at the holidays, find solace in your place of worship and break bread with your neighbors. You could have a renewed sense of confidence in our states’ leaders, knowing that we are doing what it takes to keep each other safe.
It’s important to note there’s a wide spectrum of COVID-19 tests and not all tests are created equal. The sensitivity and specificity of COVID-19 tests vary and can produce false negatives and false positive results. For example, false negatives appear in between 5 percent to 40 percent of tests. This variation can result from poor specimen collection, timing of the test (too early for detection) or faulty tests, among other factors. Testing is not foolproof. Relying on just a COVID-19 test result can give you a false sense of security, as the White House outbreak shows.
As such, even if testing is much more widely available, people should still follow basic public health protocols. An additive or layered approach is needed to reduce the risk of spread. If you’re planning to gather with family for the holidays, consider the following strategies:
Is this your picture of a normal holiday scene? Probably not. But we’re not living in normal times. Let’s keep each other safe, and do what it takes now to be able to come together for the holidays.
Former Director, Public Health Campaigns, PIRG