The foundation is crumbling
What was missing from President Obama's visionary plan for medical progress?
For months, we’ve been sharing a warning about the post-antibiotic era: it’s looming, it’s coming, it’s near… it’s here. Despite decades of knowledge that the overuse of antibiotics would lead us into a world where antibiotics no longer work, overuse has persisted. Now, we may be watching a pillar of modern medicine crumble around us.
President Obama proposed a visionary plan to cure cancer during this year’s State of the Union address, and I want to help him succeed in that mission. That’s why I’m calling attention to the dire state of our antibiotics, the foundation of modern medicine that these breakthroughs depend upon. This was the reality that tugged at my mind. Our president’s goal is commendable and, in light of the deaths of David Bowie, Alan Rickman, and thousands of others that same week due to cancer, poignant. But as antibiotics — the foundational medicines we rely on for everything from treating now-minor infections to safely conducting surgeries, and for immunosuppressive treatments like chemotherapy — begin to fail, the aura of medical discovery flickers. If the advances we’ve already made backslide, how can we move forward?
“We’re watching our demise in real time,” says Lance Price, PhD, a prominent resistance microbiologist and founder of the Antibiotic Resistance Action Center at George Washington University. As one of the leading scientists working on this issue, his sentiments are as accurate as they are sincere. Without antibiotics, illnesses we now consider minor can turn life-threatening. Methicillin-resistant Staphylococcus aureus (MRSA) infections are one such example. Staph bacteria are typically common and easily treatable with antibiotics in a matter of days. MRSA is different. Able to resist a growing number of the antibiotics we have in our arsenal, the bacteria causes infections that can be difficult, if not impossible to treat.
Almost three years ago Kristin Jackson’s toe swelled rapidly with puss, and turned dark red. She quickly realized that what she thought might have been a pulled muscle in her groin was really a massively swollen gland. Kristin decided it was time to go to the emergency room. While she sat in the hospital waiting to see the doctor she noticed that there were slight red streaks spreading from her toe up her foot and ankle. Once the doctor saw the toe he said it was most likely a MRSA infection, and that the red streaks were the infection making its way through her body. Terrified and confused, she took the prescription for the antibiotics and left. She was back to the doctor’s office shortly after with a recurring infection, and again once more. Each time they found a cocktail of antibiotics that worked to stave off the infection, but not everyone is so fortunate. MRSA infections kill an estimated 20,000 people in the U.S. each year.
Stories like Kristin’s are becoming more and more common. Evidence is mounting in support of a direct connection between farms that routinely administer antibiotics to their animals and MRSA infections in the people who live nearby. A study conducted by the Office of Veteran’s Affairs found that “the risk of MRSA nearly tripled for Veterans who lived within one mile of large pig CAFOs.” We’ve known about the risk that humans could contract antibiotic resistant infections resulting from farming practices since the 1970’s, when researchers approached the FDA about the dangers of administering routine antibiotics to livestock and poultry. Dr. Stuart Levy, director of Tuft University’s Center for Adaptation Genetics and Drug Resistance, found in 1976 that chickens fed an antibiotic called tetracycline contained tetracycline resistant organisms within one week, and those resistant bacteria spread to farmworkers that were in contact with the chickens and the feed containing the drug. The relation between superbugs and the inappropriate use of antibiotics in agriculture has only become clearer since, as researchers worldwide work to find and combat the accelerating rise of drug resistant bacteria.
The rapid rise of deadly, drug resistant infections is not a given. We can slow the rate of resistanceby stopping the practices that cause it.
Change is already occurring as consumers put their buying power behind meat raised without routine antibiotics. By voicing their concerns about the connection between factory farming and drug resistant bacteria, consumers are changing the conversation more quickly than the federal government has managed to amid attacks from the meat industry. In the last year alone, numerous major chains like McDonald’s and Subway, and producers like Tyson Foods have taken steps to reduce the use of our life-saving medicines on animals that aren’t sick. Their commitments recognize that serving meat raised without routine antibiotics isn’t just good for public health, it’s a smart business move. And you’re the one to thank for it.
It’s not won yet – to keep the industry moving forward, we’re going to convince five more major chain restaurants this year to commit to serving meat raised without routine antibiotics. To do that, we’ll need your support. Are you with us? Sign our pledge to make sure you’re kept in the loop to keep our marketplace moving towards better, safer practices that protect public health.
Topics
Authors
Bill Wenzel
Find Out More
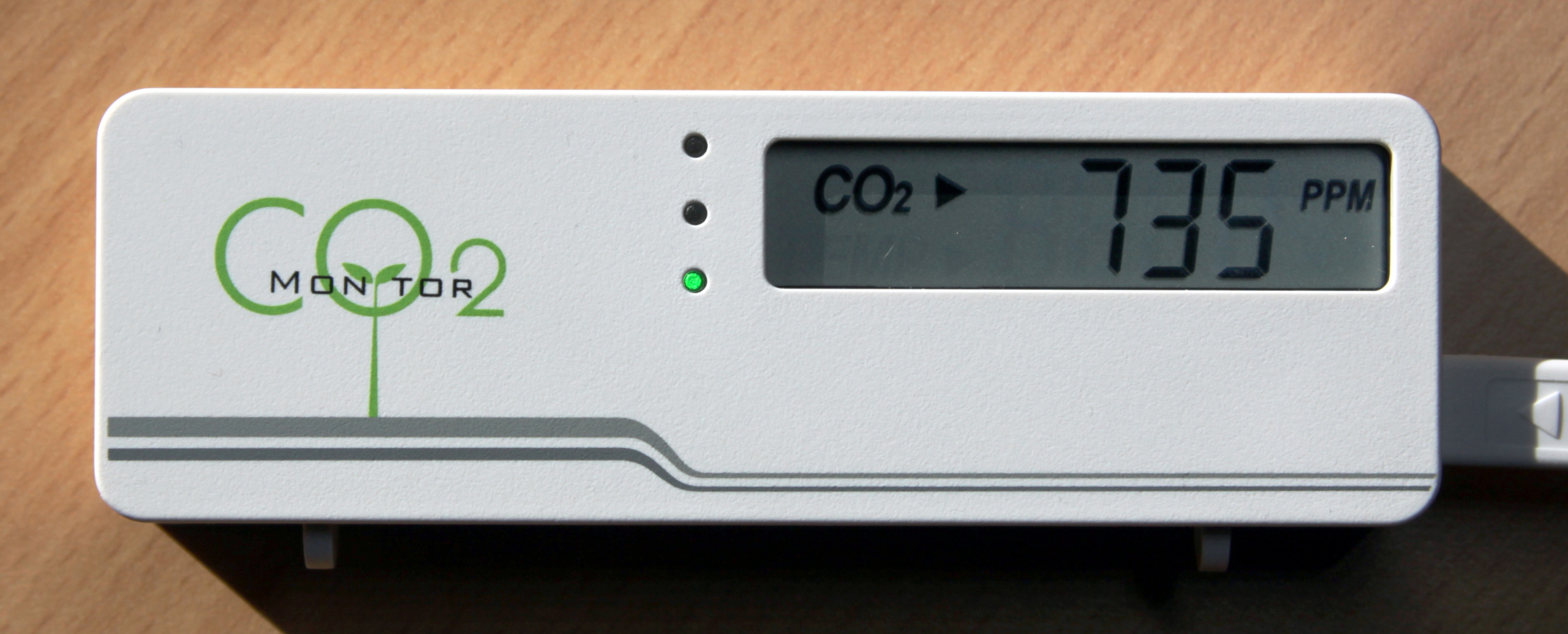
School air monitoring: A win for public health

Back to school on an electric bus

I deleted my Instagram as a teenager – here’s why