The challenge: Getting everyone vaccinated
In a separate report, the CDC said 12,702 skilled nursing facilities were enrolled in the vaccination partnership and that 90 percent of facilities, or 11,460, had at least one vaccination clinic during the first month. During those vaccination sessions, a median of 77.8 percent of residents and 37.5 percent of staff members received at least one vaccine shot. A total of 713,909 residents and 582,104 staff members received at least one shot.
The value of those first shots is clear, and the decline in cases after just the first shot isn’t surprising. While the Pfizer and Moderna vaccines require two shots weeks apart to hit the desired efficacy of 90-plus percent, both have demonstrated more than 50 percent effectiveness after just one shot in early studies.
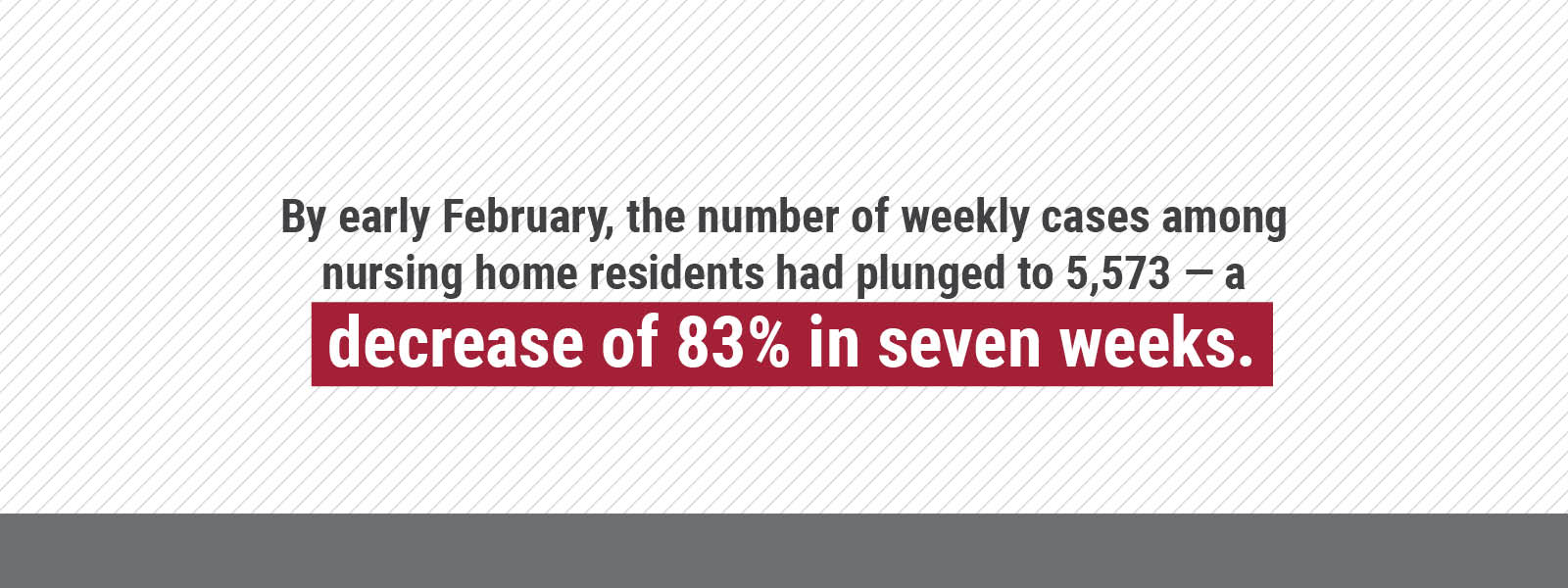
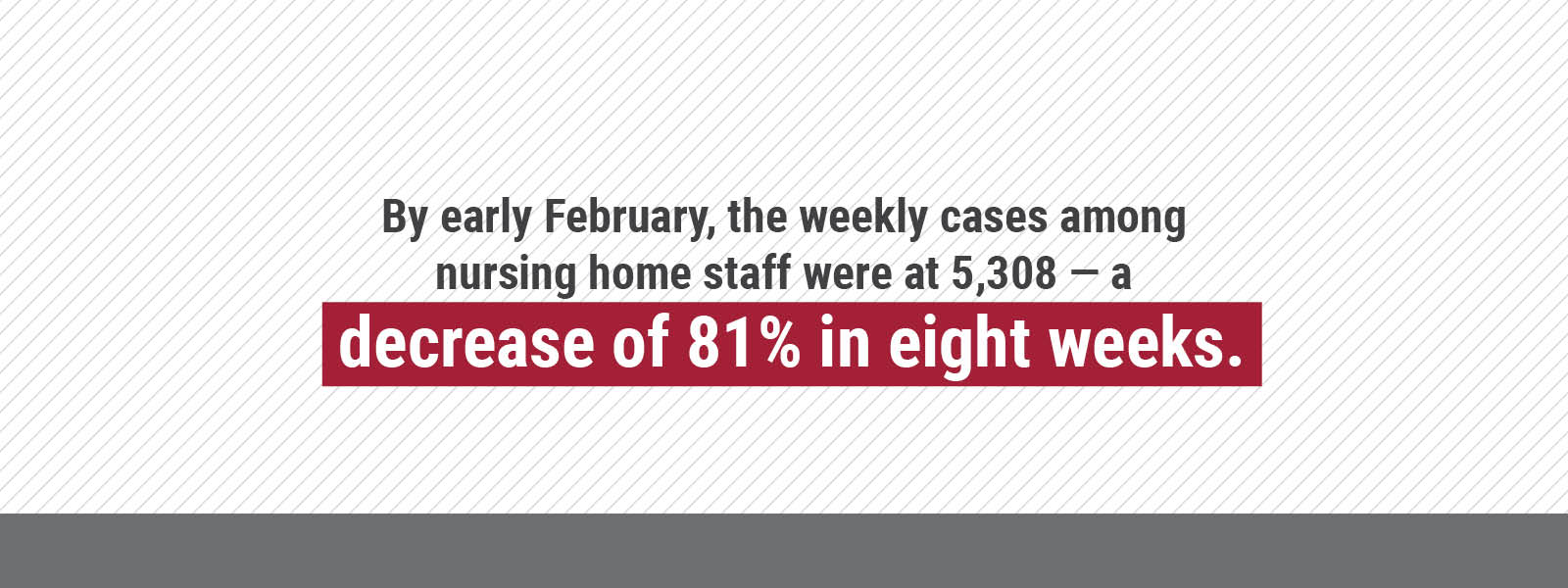
Gifford of AHCA/NCAL said researchers believe, based on the study, that vaccines may not only be preventing severe illness, but may also reduce spread. He added that nursing homes, which right now have much higher vaccination rates than the general population, are seeing cases decline at a much faster rate than in the overall population. “With the dramatic decline, it is evident the vaccine is the reason for this tremendous progress,” he said.
In its own report, the AHCA/NCAL, which represents more than 14,000 nursing homes and long term care facilities nationwide, pointed to the days around Dec. 20 — when vaccinations started — as the time when things changed for the better.
Further, the AHCA/NCAL is encouraging more staff to get vaccinated, because nursing homes still face risks and the vaccines work, AHCA/NCAL President and CEO Mark Parkinson said in a statement.
“The rapid decline of nursing home cases is incredibly encouraging and a major morale boost for frontline caregivers who have been working tirelessly for a year to protect our residents,” Parkinson said. “We hope this will help persuade those staff members who preferred to wait and see how the vaccines went that they are safe and effective, and that by each of us doing our part, we can save lives.
“I’ve long said there is a light at the end of the tunnel, but we still have a long road ahead. The more of us that receive the vaccine, the quicker we can end the pandemic and be together again.”
The AHCA is working with the CDC on a #GetVaccinated campaign, financed in part by the CDC. Its website, getvaccinated.us, includes medical information from respected medical professionals and scientists and urges vaccinated staff to share their personal experiences on social media. Its goal is to get 75 percent of staff vaccinated by June 30.