Protect public health workers and all Americans
Call on your Representatives in Congress to support more COVID funding for nursing homes.
Thousands of nursing homes nationwide are dealing with horrific shortages of masks, gowns and other items they need to protect residents, workers and the broader community from COVID-19. And seven months into this pandemic, the shortages have actually become much worse.
A report created as part of a series by U.S. PIRG Education Fund and Frontier Group
By Teresa Murray, U.S. PIRG Education Fund, and Jamie Friedman, Frontier Group
DOWNLOAD THE REPORT
Thousands of nursing homes nationwide are dealing with horrific shortages of masks, gowns and other items they need to protect residents, workers and the broader community from COVID-19. And seven months into this pandemic, the shortages have actually become much worse.
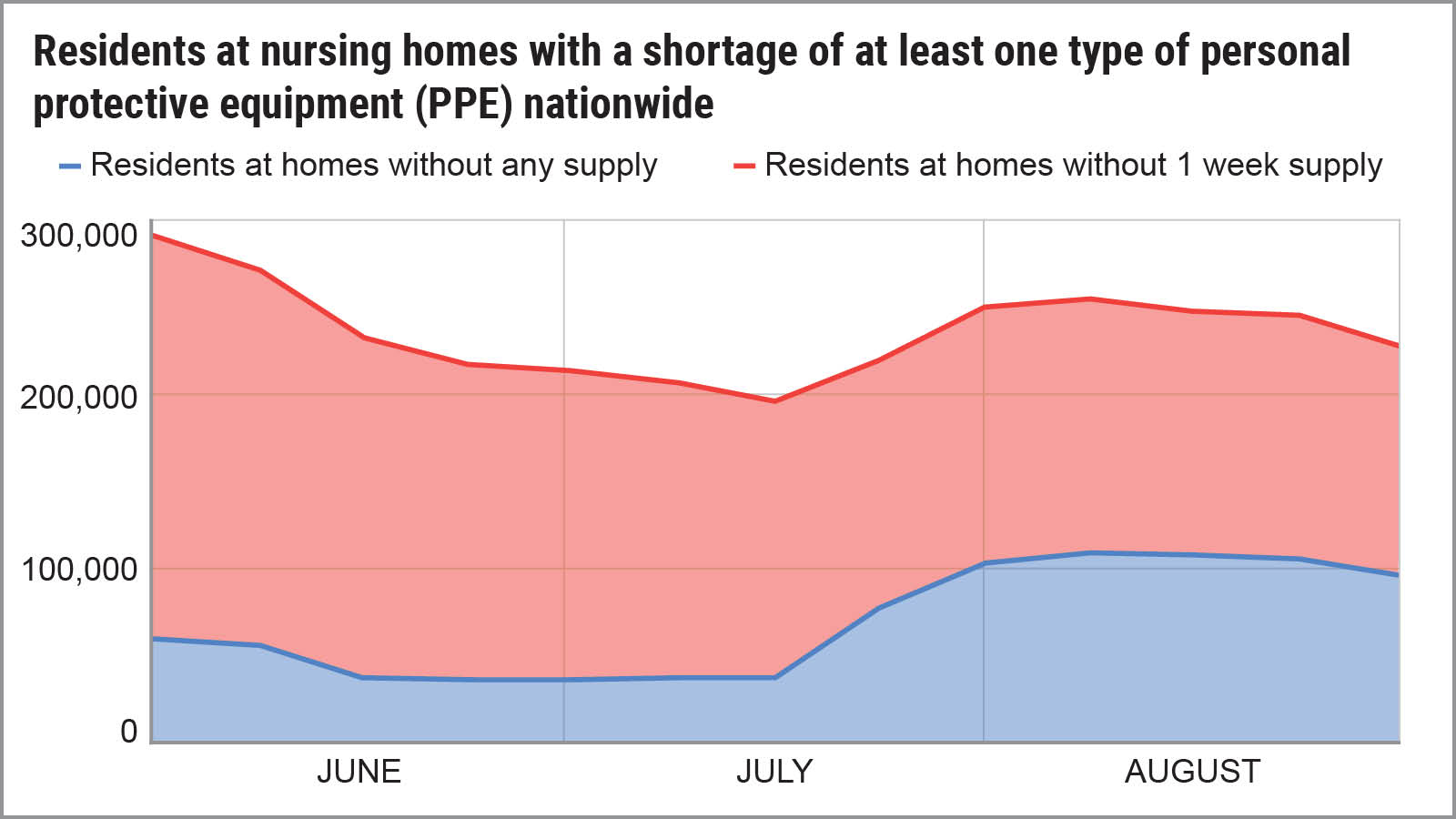
At any given time, about 1.3 million people with long-term medical issues or short-term rehabilitation needs are residing in the nation’s 15,000 nursing homes. And too many of them are at risk, according to an analysis of government data by U.S. PIRG Education Fund and Frontier Group.

Source: U.S. PIRG / Frontier Group analysis of data from data.CMS.gov

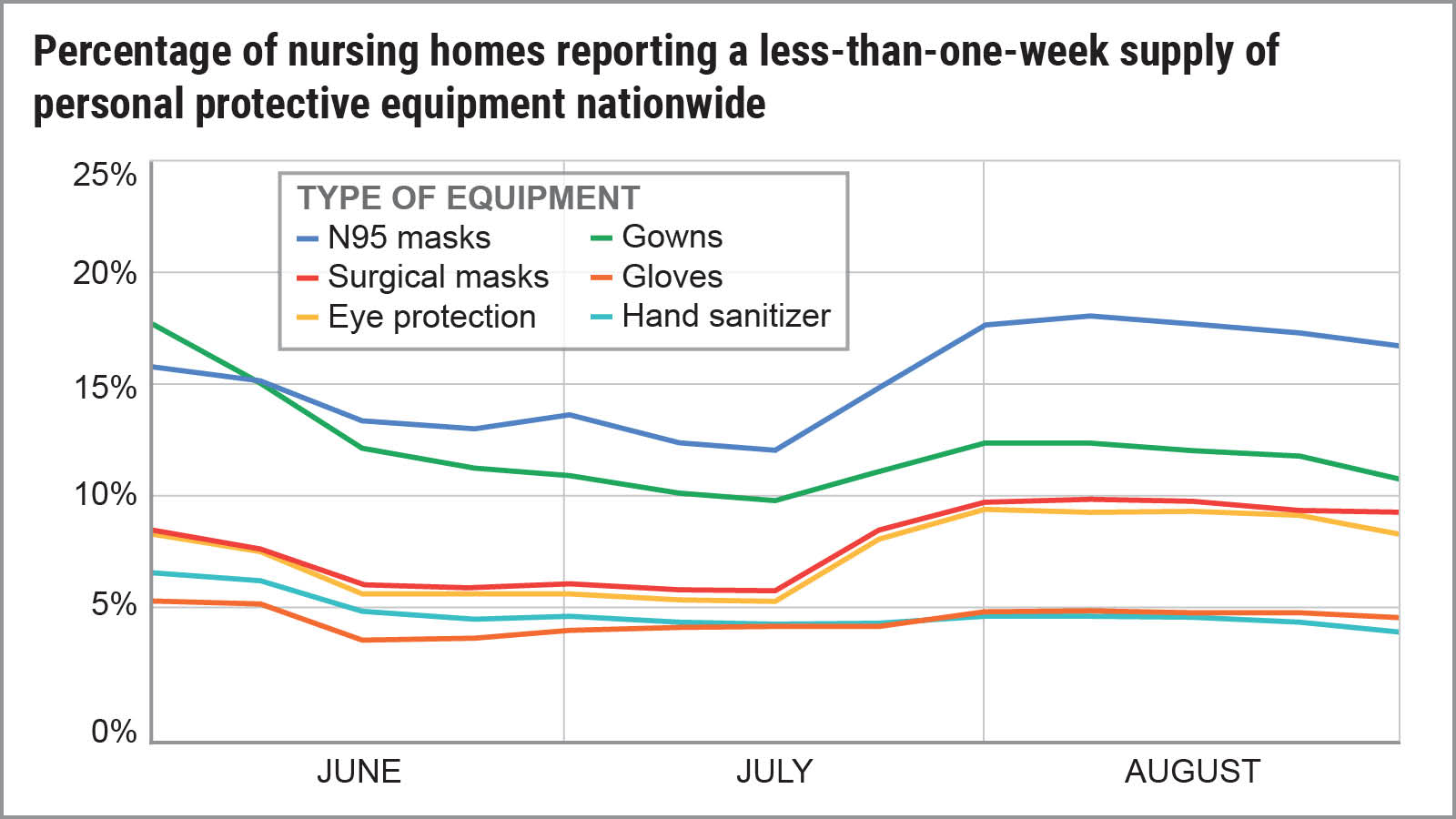
As of late August, 226,495 residents in 2,981 nursing homes nationwide were at risk because the homes had dangerously low supplies of one or more types of personal protective equipment (PPE) such as N95 masks or gowns, according to data submitted to the federal government. That means that 20 percent of nursing homes in late August had a less-than-one-week supply of one or more types of PPE, which represents a critical shortage by industry standards.
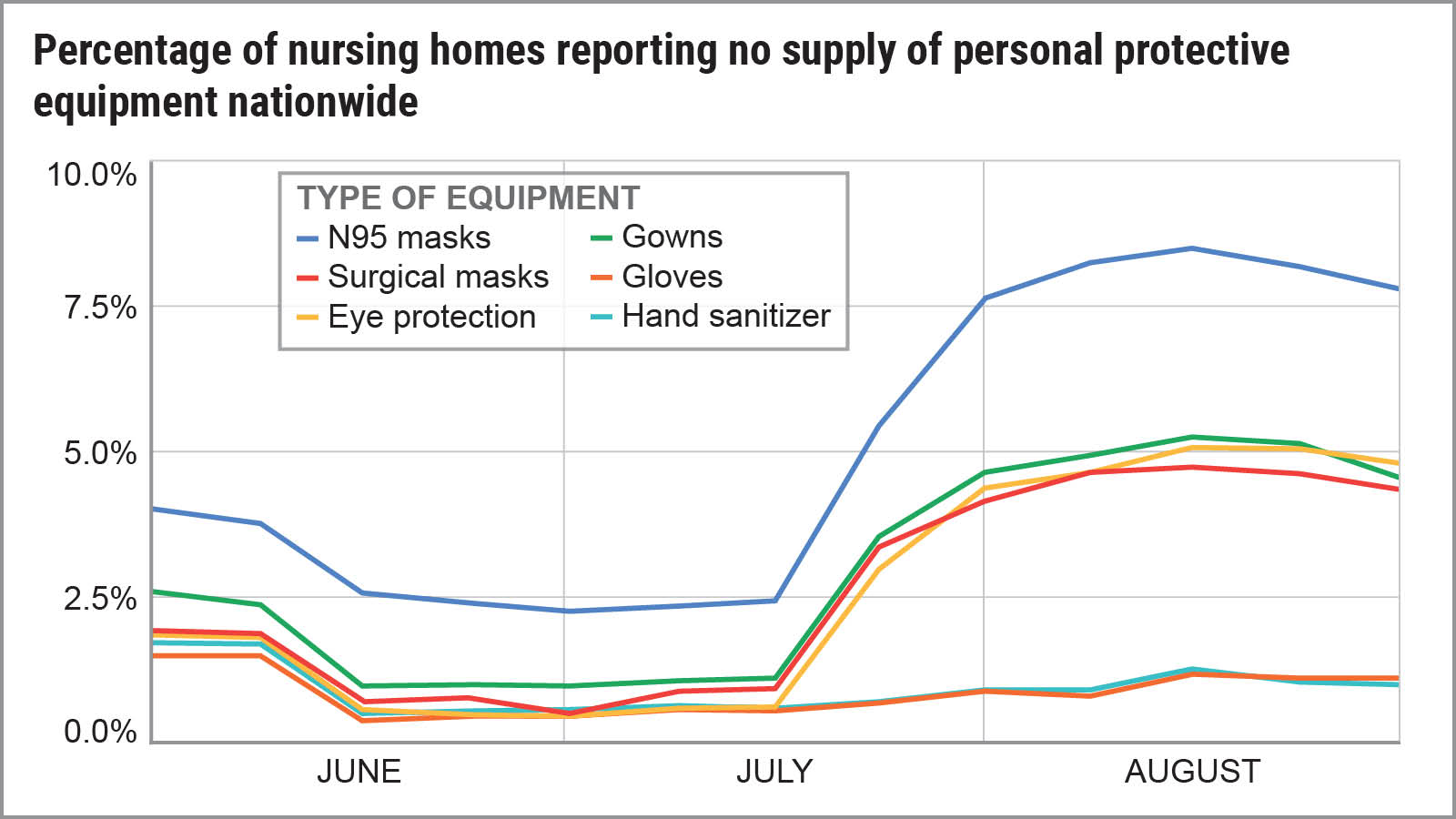
The shortages actually became more grave as the summer went on, with three times as many nursing homes reporting they were completely out of masks, gowns and eye protection in late August, compared with mid-July.

Source: U.S. PIRG / Frontier Group analysis of data from data.CMS.gov

Forty-six percent of all nursing homes nationwide reported they didn’t have a one-week supply of at least one type of PPE at some point from May through August. A one-week supply is considered the minimum acceptable. If a home has an outbreak, it can burn through its limited supply in a day or two. In addition, a home may have no idea when its next shipment of PPE may arrive. Homes with less than one week’s supply often ration, forcing workers to re-use PPE or go without.
In January, the U.S. government declared a public health emergency in response to the global threat from the coronavirus. Yet seven months after the public health emergency declaration, this nation was still experiencing dangerous shortages of PPE.

Heightened danger in nursing homes
It’s not entirely surprising that while nursing homes contain less than one-half of 1 percent of the U.S. population, they’ve produced 3 percent of the nation’s COVID-19 cases and 27 percent of deaths.
Experts believe nursing homes have been hit harder in part because the living space is tighter, residents are there around-the-clock, and people in nursing homes and rehabilitation facilities are generally older and in poorer health than the overall population. Certainly, the PPE shortages have made difficult situations even worse.
Workers are generally expected to change their PPE before every new patient to avoid potentially transferring the coronavirus from one patient to another.
“The consequences are devastating,” said Dr. David Gifford, chief medical officer at the American Health Care Association/National Center for Assisted Living (AHCA/NCAL), the nation’s largest industry association. “Long-term care is not a profession where social distancing is possible — caregivers must closely interact with their patients and residents to provide the utmost care.”

Source: U.S. PIRG / Frontier Group analysis of data from data.CMS.gov

The impact of PPE shortages? It goes beyond putting individual patients at risk. Experts say:

What’s behind the shortages?
It’s clear the nation as a whole didn’t have adequate amounts of PPE to handle a once-in-a-century global pandemic. (No explanations have been provided about why the Strategic National Stockpile under the U.S. Department of Health and Human Services didn’t have more supplies.)
Nursing homes usually buy PPE individually through third-party suppliers, the AHCA said. But the supply chain has been completely disrupted this year. “During this pandemic, providers were desperate for PPE, creating their own or even trying to buy it off Amazon,” Gifford said.
Overall, the shortages were more severe in some states because of myriad reasons: outbreaks, economics, poor planning, politics or some combination of those.

Why is the situation so bad in nursing homes?
Demand for PPE is coming from every sector of the economy, not just health care. The world supply chain was strained. The AHCA begged the federal and state governments to help nursing homes and assisted living centers, Gifford said. But long-term care facilities weren’t prioritized to receive PPE, he said.
Robyn Grant, director of public policy and advocacy at the nonprofit National Consumer Voice for Quality Long-Term Care, said the U.S. government didn’t provide much help: a two-week supply of PPE. In addition, a number of facilities reported that some of the PPE was defective, including gowns with no arm holes and expired N95 masks, Grant said.
As bad as it was in the spring, it got worse, with PPE shortages skyrocketing in nursing homes in mid-July. Experts blame three phenomena: the reopening of restaurants and other businesses in many states in June and July; outbreaks in the South as people flocked to vacation spots and started enjoying summer fun; and the resumption of activities within other medical businesses such as elective surgeries, in-person doctor’s appointments and veterinary procedures.
The PPE shortages exist across various health care settings, according to the American Nurses Association (ANA), which in September released a survey of 21,000 nurses nationwide. Forty-two percent of them said they continue to cope with “widespread or intermittent” shortages of PPE.
PPE shortages in nursing homes put residents and staff at greater risk of getting the virus and spreading it, Grant said.
“We have heard staff say that they have been required to use one mask for days, and that in some cases they have had to use garbage bags because there weren’t enough gowns,” she said. “We’ve also heard staff talk about how worried they are about taking the virus back home to their loved ones.” Reusing a mask violates health care protocols.

This crisis isn’t going away without action
We face the possibility of a brutal fall and winter if another wave of COVID-19 combined with a normal flu season further strains PPE supplies. Three months ago, a 25-member commission of non-partisan experts, organized by the Centers for Medicare & Medicaid Services, issued urgent warnings that the problem will become more dire. In its updated report in September, the Coronavirus Commission on Safety and Quality in Nursing Homes said homes continue to be plagued by shortages in PPE, as well as testing and staffing shortages.
“Additional federal action is necessary to ensure sufficient availability of high-quality testing and PPE,” the commission wrote. “Without this, and related training, the virus will continue to spread.”
Here’s what’s needed:
Something must change soon. “Our health care heroes are risking their own safety and security to continue their valiant work of caring for our nation’s most vulnerable,” Gifford said. “And we must rally around them and our vulnerable residents.”
Call on your Representatives in Congress to support more COVID funding for nursing homes.
Sign Up

Video guides
How to find information (PPE shortages, staff shortages, outbreaks, etc.) about a specific nursing home.

How to look up all nursing homes in a particular city, zip code.
